The Lancet Global Health Oxygen Commission
It’s here! Two and half years in the making, The Lancet Global Health Commission on Medical Oxygen Security released its report on 17 February 2025. You can find the full Commission report and Comments here and related documents below including:
- Media Statement
- Presentation Deck
- Policy briefs in English, French, Spanish, Russian, Chinese, and Arabic.
- Spotlight briefs:
- Country Case Studies from Bangladesh, India, Malawi, Nigeria, Sweden, and Uganda.
- Video testimonials from Saude Abdullahi (Nigeria), Baby Ahammad’s Family (Bangladesh), Aggrey Aluso (Kenya), Nomawethu Jele (South Africa), Blessi Kumar (India), and Maurine Murenga (Kenya) here.
- Don’t miss the podcast interview with The Lancet Global Health editor-in-chief Zoë Mullan and two of the Commission authors, Dr Carina King and Dr Ehsan Rahman, here.
- All of the evidence that informed the Commission is now available in the A2O2 Resource Library, hosted by PATH here!
Who led The Lancet Global Health Oxygen Commission?
The Commission was overseen by 18 Commissioners – academic experts representing all regions – and 40 Advisors provided guidance, supported by an Executive Committee including Makerere University (Uganda), icddr,b (Bangladesh), the University of Melbourne/Murdoch Children’s Research Institute (Australia), the Karolinska Institutet (Sweden), and the Every Breath Counts Coalition (USA). The Commission also engaged regularly with a global network of Oxygen Access Collaborators and conducted interviews with patients, caregivers, and clinicians and consultations with governments and industry.
Why did we need a commission?
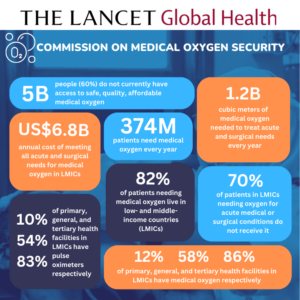
Medical oxygen is an essential medicine with no substitute for the treatment of at least 20 Global Burden of Disease conditions, including HIV/AIDS, TB, malaria, pneumonia, COVID-19, maternal and neonatal disorders, tracheal, bronchus, and lung cancers, anemia, sickle cell disease, heart disease, stroke, COPD, asthma, transport injuries, poisonings, foreign body injuries, self-harm, and interpersonal violence. Together, these conditions caused a massive 40 million deaths in 2021, almost 60% of all human deaths.
Medical oxygen is particularly lifesaving for newborns and children. A recent review found that deaths among hospitalized children fell by 25% when pulse oximetry and oxygen was provided, and that oxygen is as cost-effective as childhood vaccination. But oxygen is often unavailable in health facilities, especially those located in low- and middle-income countries (LMICs). And where it is available, it is often unaffordable leaving the most vulnerable patients without access to a lifesaving medicine.
COVID-19 exposed a tragic gap
Lack of medical oxygen was a defining inequity of the COVID-19 pandemic, with LMICs bearing the brunt of oxygen shortages and related deaths. The pandemic exposed not only a tragic gap in inadequate supplies of medical oxygen and respiratory therapies, but also the trained workforce needed to install, operate, and maintain the lifesaving equipment. The gap had always been there – contributing to a massive burden of death that was largely hidden. When COVID-19 unleashed a new wave of patients needing oxygen, hospitals were unable to meet the demand and the world watched as patients died waiting for oxygen on gurneys in the parking lots of hospitals, in the backseats of cars, and at home waiting for loved ones to return with filled cylinders.
A study of COVID-19 deaths in 64 intensive care units across 10 African countries showed that one in two patients died without receiving medical oxygen, and a study from Peru, which recorded the highest COVID-19 death rate in the world, found that oxygen saturation below 90% on admission was a strong predictor of mortality. The authors concluded that in settings with limited resources, efforts to reduce COVID-19 deaths should focus on early identification of hypoxemia and timely access to oxygen.
Oxygen gaps remain in many countries
Despite the additional oxygen supplies many countries received during the pandemic, including US$1 billion from the ACT-Accelerator Oxygen Emergency Taskforce, access gaps remain. Many governments still do not know how much oxygen their health systems need to meet the needs of patients during routine times, or how much surge capacity will be needed when the next respiratory pandemic strikes. Likewise, global health partners are in the dark about how much, and what kind, of oxygen support different countries need to strengthen their health systems most cost-effectively.
The Lancet Global Health Commission on Medical Oxygen Security is a major effort to change this. Announced in September 2022, the Commission sheds light onto the number of patients needing medical oxygen each year in each region and the cost of meeting that need, how to define and measure oxygen coverage, which oxygen solutions work best in different settings, and how to generate the financing and political will to achieve transformational change. It addresses all levels of care from hospital to home, all age groups from neonates to the elderly, all health conditions where oxygen is a recommended treatment, and all the ways in which access to oxygen can contribute to health system strengthening and pandemic preparedness.
Promising new developments
Governments and global health and development agencies urgently need this information as they pivot from pandemic response to preparing for the next crisis and return to the job of achieving the Sustainable Development Goals. The new Global Oxygen Alliance (GO₂AL), co-chaired by The Global Fund and Unitaid, and the World Health Organization’s Increasing Access to Medical Oxygen Resolution, endorsed by all 194 Member States, are both welcome additions to the global health architecture and vital to the successful implementation of the Commission’s recommendations.
Watch the 18 February 2025 official global launch of The Lancet Global Health Oxygen Commission here and read the report here.
- Learn about the Commission’s key findings and 52 recommendations, including the size of medical oxygen coverage gaps and the cost of closing them.
- Discover the Commission’s new tools, including an Access to Medical Oxygen Scorecard (ATMO₂S), 10 Oxygen Coverage Indicators, 20 Priority Areas for Oxygen Innovation, and more.
- Join the global effort to ensure that no more patients die for lack of access to oxygen – an essential medicine to save lives now and during future public health emergencies like COVID-19.
Regional Launches
- South Asia, Regional World Health Summit, 27 April, New Delhi, with One Health Trust, WHO SEARO, PATH, National Neonatology Forum, Global Coalition of TB Advocates, and more.

- Western Pacific, Australian Global Health Alliance 2025 Congress, 2 April, Sydney, represented by lead Commission author Hamish Graham from the University of Melbourne and the Murdoch Children’s Research Institute below.

- North America, Consortium of Universities for Global Health (CUGH) Annual Conference, 20 February, Atlanta, represented by Oxygen Commissioner Shams Arifeen (below) and author Dr Ehsan Rahman from icddr,b.

Reactions
Read what stakeholders are saying about the Commission and how they are advancing implementation of its recommendations:
- Global Oxygen Alliance (GO₂AL), March 2025
- Sanrai International, March 2025
- PATH, February 2025
- One Health Trust, February 2025
- Murdoch Children’s Research Institute (MCRI), February 2025
RESOURCES
Events
- North American launch (in-person only) of The Lancet Global Health Oxygen Commission at the Consortium of Universities for Global Health (CUGH), 20 February, 2025. Register here. Learn more about the special workshop here
- World Health Summit Global Health Lab, 15 October 2024, to preview the findings of the Commission, with representatives from government, global health agencies, academia, industry, and civil society. Watch the recording here
Media
- Why over 5 billion people still lack access to life-saving medical oxygen, News Medical Life Sciences, 23 February, 2025
- The global oxygen crisis, BBC Health Check, 20 February, 2025
- An Invisible Medical Shortage: Oxygen, New York Times, 18 February, 2025
- Stifled Oxygen Access, Global Health Now, 18 February, 2025
- Medical oxygen in short supply in many parts of world, The Hill, 18 February, 2025
- Report: Improving oxygen access, pandemic preparedness could save millions of lives, CIDRAP, 18 February, 2025
- Five billion people lack access to safe, affordable medical oxygen globally, Nigerian Tribune, 17 February, 2025
- 60% world population lacks access to medical oxygen, Vanguard Nigeria, 18 February, 2025
- A Global Oxygen Crisis Is Putting Millions of Lives at Risk, Science Alert, 19 February 2025
- 5 billion globally lack access to medical oxygen, poor nations most affected: Lancet report, The Economic Times, 18 February, 2025
- Post-Covid lessons not learnt: Lancet flags five billion people still lack access to medical oxygen, The Indian Express, 20 February, 2025
Statements
- Commissioner Call to Action for World Oxygen Day, 2 October 2024 (Spanish)
- Milestone Medical Oxygen Meeting an Opportunity for Countries to Make Rapid Progress on Access, 10 May 2024
- UN General Assembly Lancet Global Health Oxygen Commission Statement, 15 September 2023 (French) (Spanish)
- Milestone Adoption of Medical Oxygen Resolution & Launch of new Global Oxygen Alliance at the World Health Assembly, 26 May 2023
- WHO Oxygen Resolution a Major Milestone for Access to Medical Oxygen, Every Breath Counts, 3 February 2023
- Welcoming the Lancet Global Health Commission on Medical Oxygen Security, Every Breath Counts, 25 September 2022
- Announcing the Lancet Global Health Commission on Medical Oxygen Security, Lancet Global Health, 23 September 2022
Latest from the Commissioners, Advisors, and Executive Committee
- Leith Greenslade, Expanding Medical Oxygen Access Without U.S. Foreign Aid, Think Global Health, March 2025
- David Lowrance, et al, A rapid facility-level assessment of oxygen systems in 39 low-income and middle-income countries: a cross-sectional study, Lancet Global Health, February 2025
- Adegoke Falade with Rami Subhi, Towards equity: the unfinished crisis of medical oxygen, Lancet Global Health, February 2025
- Ramanan Laxminarayan, Reducing global inequities in medical oxygen access: the Lancet Global Health Commission on medical oxygen security, One Health Trust, February 2025
- Lisa Smith, Report on medical oxygen finds a 70 percent coverage gap and calls for action to end suffering and death, PATH, February 2025
- Hamish Graham, Global action needed to solve the medical oxygen crisis, Murdoch Children’s Research Institute, February 2025
- Steve Howie with Sainimere Boladuadua, Widespread suffering and death from lack of medical oxygen, University of Auckland, February 2025
- Tim Baker, Lack of access to medical oxygen is causing widespread suffering and death, Essential Emergency and Critical Network, February 2025
- Hamish Graham, Putting Oxygen Access on the Global Health Agenda, Regional World Health Summit, May 2024
- Neelima Navuluri, Filling the Oxygen Gap. Patients in low-income countries often aren’t getting adequate medical oxygen, a new DGHI-led study reveals, February 2024, based on Prevalence and phenotypic trajectories of hypoxaemia among hospitalised adults in Kenya: a single-centre, prospective cohort study, BMJ Respiratory Medicine, September 2023
- Lisa Smith, et al, Variability of oxygen requirements in critically ill COVID-19 patients, Journal of Global Health, February 2024
- Shams el Arifeen, et al, Implementation of bubble continuous positive airway pressure for children with severe pneumonia and hypoxemia in intensive care unit of Dhaka Hospital, Bangladesh, Pediatric Pulmonology, January 2024
- Ramanan Laxminarayan with Varun Manhas, National Medical Oxygen Grid, October 2022, Overview Deck, and Letter of Support from Madhya Pradesh Government, January 2024
- Hamish Graham, Freddy Kitutu, Freddie Ssengooba, Felix Lam, et al, Improving Effective Coverage of Medical Oxygen Services For Neonates and Children in Health Facilities in Uganda: A Before-After Interventional Study, The Lancet Preprint, December 2023
- Tisugane Mvalo, Eric McCollum, et al, A hidden pandemic: the danger of donated respiratory devices to children in LMICs, Lancet Global Health, December 2023
- Heather Zar and Eric McCollum, Pulse oximetry to detect paediatric hypoxaemia-the fifth vital sign, Lancet Global Health, November 2023
- Ramanan Laxminarayan and Leith Greenslade, Solving for Oxygen, Think Global Health, September 2023
- Robert Matiru with Zachary Katz, Opinion: Adopting WHO’s oxygen resolution is imperative to save lives, Devex, March 2023
Climate change and respiratory health
Climate Change and Respiratory Health, brought together four leading experts – Heather Adair-Rohani from the World Health Organization (WHO), Rebecca Nantanda from Makerere University Lung Institute, Laura-Jane Smith from the British Thoracic Society, and John Sampson from Johns Hopkins University to explore different facets of...
11 December, 2024Open Letter to The Global Fund Board: Access to medical oxygen
Dear Global Fund Board, The Global Fund must continue its vital work helping eligible countries close the massive gaps in access to medical oxygen that are stymying efforts to achieve the Sustainable Development Goals (SDGs) and prepare for the next pandemic. Oxygen is an essential...
19 November, 2024Medical oxygen and the SDGs
“Apart from oxygen, name one other essential medicine that is a topline treatment for all but one of the conditions targeted by the health SDGs?” This was the focus of the second of three High Stakes Conversations on the role of medical oxygen and global...
09 July, 2024What do the new Global Burden of Disease estimates tell us about childhood pneumonia?
For the first time since global child mortality statistics have been collected, the end of child pneumonia deaths is in sight. New estimates from the Global Burden of Diseases, Injuries, and Risk Factors Study (GBD) show that the number of children dying from pneumonia dropped...
21 May, 2024Medical oxygen and respiratory pandemics
This was the focus of the first of three High Stakes Conversations on the role of medical oxygen and respiratory therapies hosted by Every Breath Counts on 30 April 2024. The event, Respiratory Pandemics and Access to Medical Oxygen, brought together four leading experts on...
12 May, 2024The promise of reduced dose pneumococcal vaccination for children
Pneumonia is the leading infectious cause of death in children under five and, as a result, the pneumococcal conjugate vaccine, or PCV, is one of the most lifesaving vaccines. However, just six in every ten children are protected with PCV well below the global target...
17 March, 2024